“And where there is a scientific vacuum, drug companies are happy to insert a marketing message and call it science. As a result, psychiatry has become a proving ground for outrageous manipulations of science in the service of profit.”- Dr. Daniel Carlat
“Depression is a serious medical condition that may be due to a chemical imbalance, and Zoloft works to correct this imbalance.”
Herein lies the serotonin myth.
As one of only two countries in the world that permits direct to consumer advertising, you have undoubtedly been subjected to promotion of the “cause of depression.” A cause that is not your fault, but rather; a matter of too few little bubbles passing between the hubs in your brain! Don’t add that to your list of worries, though, because there is a convenient solution awaiting you at your doctor’s office…
What if I told you that, in 6 decades of research, the serotonin (or norepinephrine, or dopamine) theory of depression and anxiety has not achieved scientific credibility?
You’d want some supporting arguments for this shocking claim.
So, here you go:
The Science of Psychiatry is Myth
Rather than some embarrassingly reductionist, one-deficiency-one-illness-one-pill model of mental illness, contemporary exploration of human behavior has demonstrated that we may know less than we ever thought we did. And that what we do know about root causes of mental illness seems to have more to do with the concept of
evolutionary mismatch than with genes and chemical deficiencies.
In fact, a
meta-analysis of over 14,000 patients and Dr. Insel, head of the NIMH, had this to say:
“Despite high expectations, neither genomics nor imaging has yet impacted the diagnosis or treatment of the 45 million Americans with serious or moderate mental illness each year.”
To understand what imbalance is, we must know what balance looks like, and neuroscience, to date, has not characterized the optimal brain state, nor how to even assess for it.
A
New England Journal of Medicine review on Major Depression, stated:
” … numerous studies of norepinephrine and serotonin metabolites in plasma, urine, and cerebrospinal fluid as well as postmortem studies of the brains of patients with depression, have yet to identify the purported deficiency reliably.”
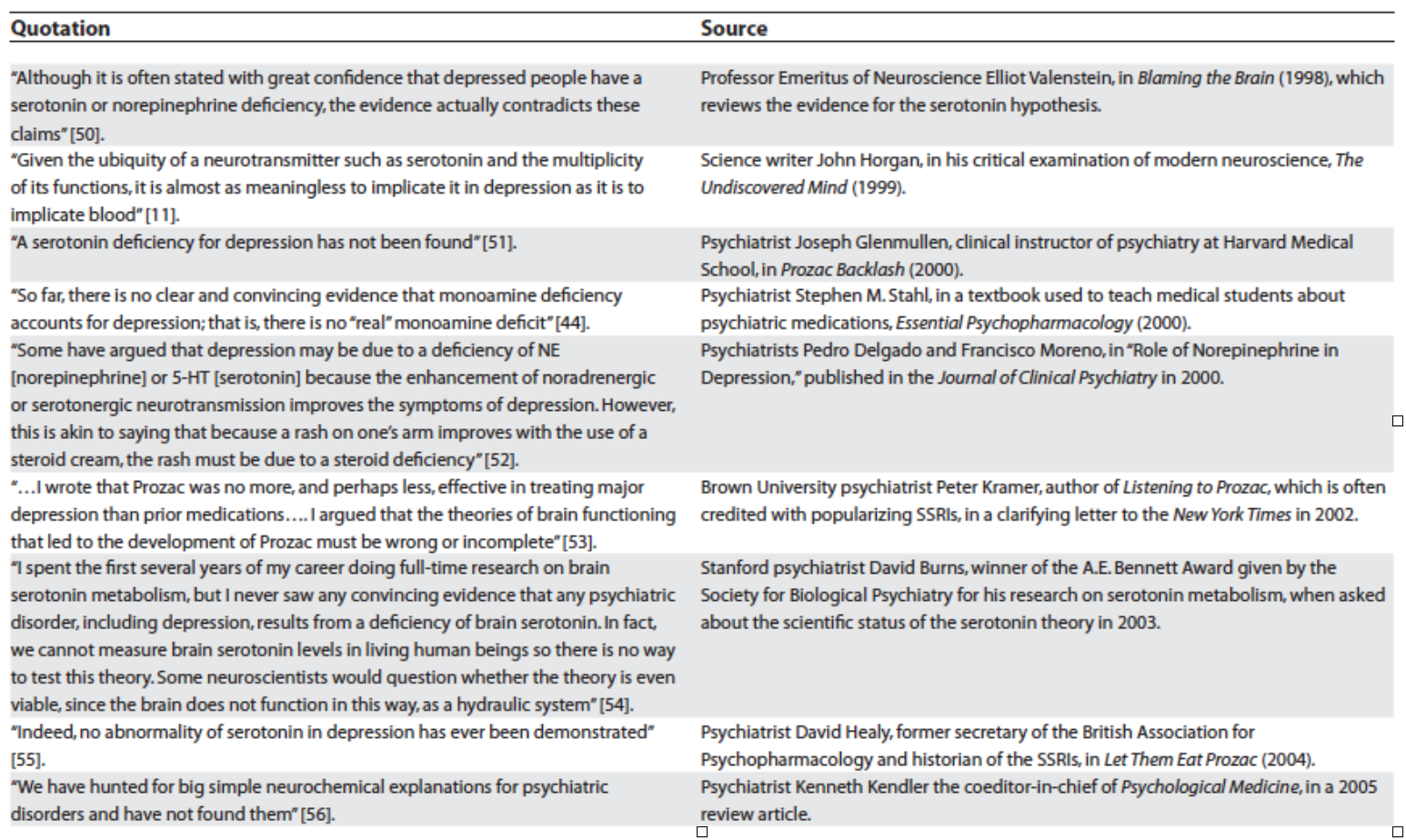
The data has poked holes in the theory and even the field of psychiatry itself is putting down its sword. One of my favorite
essays by Lacasse and Leo has compiled sentiments from influential thinkers in the field – mind you, these are conventional clinicians and researchers in mainstream practice – who have broken rank, casting doubt on the entirety of what psychiatry has to offer around antidepressants:
Humble Origins of a Powerful Meme
In the 1950s, reserpine, initially introduced to the US market as an anti-seizure medication, was noted to deplete brain serotonin stores in subjects, with resultant lethargy and sedation. These observations colluded with the clinical note that an anti-tuberculosis medication, iproniazid, invoked mood changes after five months of treatment in 70% of a 17 patient cohort. Finally, Dr. Joseph Schildkraut threw fairy dust on these mumbles and grumbles in 1965 with his hypothetical manifesto entitled “The Catecholamine Hypothesis of Affective Disorders” stating:
“At best, drug-induced affective disturbances can only be considered models of the natural disorders, while it remains to be demonstrated that the behavioral changes produced by these drugs have any relation to naturally occurring biochemical abnormalities which might be associated with the illness.”
Contextualized by the ripeness of a field struggling to establish biomedical legitimacy (beyond the therapeutic lobotomy!), psychiatry was ready for a rebranding, and the pharmaceutical industry was all too happy to partner in the effort.
Of course, the risk inherent in “working backwards” in this way (noting effects and presuming mechanisms) is that we tell ourselves that we have learned something about the body, when in fact, all we have learned is that patented synthesized chemicals have effects on our behavior. This is referred to as the
drug-based model by
Dr. Joanna Moncrieff. In this model, we acknowledge that antidepressants have effects, but that these effects in no way are curative or reparative.
The most applicable analogy is that of the woman with social phobia who finds that drinking two cocktails eases her symptoms. One could imagine how, in a 6 week randomized trial, this “treatment” could be found efficacious and recommended for daily use and even prevention of symptoms. How her withdrawal symptoms after 10 years of daily compliance could lead those around her to believe that she “needed” the alcohol to correct an imbalance. This analogy is all too close to the truth.
Running With Broken Legs
Psychiatrist Dr. Daniel Carlat has said:
“And where there is a scientific vacuum, drug companies are happy to insert a marketing message and call it science. As a result, psychiatry has become a proving ground for outrageous manipulations of science in the service of profit.”
So, what happens when we let drug companies tell doctors what science is? We have an industry and a profession working together to maintain a house of cards theory in the face of contradictory evidence.
We have a
global situation in which increases in prescribing are resulting in increases in severity of illness (including numbers and length of episodes) relative to those who have never been treated with medication.
To truly appreciate the breadth of evidence that states antidepressants are ineffective and unsafe, we have to get behind the walls that the pharmaceutical companies erect. We have to unearth unpublished data, data that they were hoping to keep in the dusty catacombs.
A now famous
2008 study in the
New England Journal of Medicine by Turner et al sought to expose the extent of this data manipulation. They demonstrated that, from 1987 to 2004, 12 antidepressants were approved based on 74 studies. Thirty-eight were positive, and
37 of thesewere published. Thirty-six were negative (showing no benefit), and
3 of these were published as such while 11 were published with a
positive spin (always read the data not the author’s conclusion!), and 22 were unpublished.
In 1998 tour de force, Dr. Irving Kirsch, an expert on the placebo effect, published a
meta-analysis of 3,000 patients who were treated with antidepressants, psychotherapy, placebo, or no treatment and found that only 27% of the therapeutic response was attributable to the drug’s action.
This was followed up by a 2008
review, which invoked the Freedom of Information Act to obtain access to unpublished studies, finding that, when these were included, antidepressants outperformed placebo in only 20 of 46 trials (less than half!), and that the overall difference between drugs and placebos was 1.7 points on the 52 point Hamilton Scale. This small increment is clinically insignificant, and likely accounted for by medication side effects strategically employed (sedation or activation).
When active placebos were used, the
Cochrane database found that differences between drugs and placebos disappeared, given credence to the assertion that inert placebos inflate perceived drug effects.
The finding of tremendous placebo effect in the treatment groups was also echoed in two different meta-analyses by
Khan et al who found a 10% difference between placebo and antidepressant efficacy, and comparable suicide rates. The most
recent trial examining the role of “expectancy” or belief in antidepressant effect, found that patients lost their perceived benefit if they believed that they might be getting a sugar pill even if they were continued on their formerly effective treatment dose of Prozac.
The largest, non-industry funded
study, costing the public $35 million dollars, followed 4000 patients treated with Celexa (not blinded, so they knew what they were getting), and found that half of them improved at 8 weeks. Those that didn’t were switched to Wellbutrin, Effexor, or Zoloft OR “augmented” with Buspar or Wellbutrin.
Guess what? It didn’t matter what was done, because they remitted at the same unimpressive rate of 18-30% regardless with only 3% of patients in remission at 12 months.
How could it be that medications like Wellbutrin, which purportedly primarily disrupt dopamine signaling, and medications like Stablon which theoretically enhances the reuptake of serotonin, both work to resolve this underlying imbalance? Why would thyroid, benzodiazepines, beta blockers, and opiates also “work”? And what does depression have in common with panic disorder, phobias, OCD, eating disorders, and social anxiety that all of these diagnoses would warrant the same exact chemical fix?
Alternative options
As a holistic clinician, one of my bigger pet peeves is the use of amino acids and other nutraceuticals with “serotonin-boosting” claims. These integrative practitioners have taken a page from the allopathic playbook and are seeking to copy-cat what they perceive antidepressants to be doing.
The foundational “data” for the modern serotonin theory of mood utilizes tryptophan depletion methods which involve feeding volunteers amino acid mixtures without tryptophan and are rife with complicated interpretations.
Simply put, there has never been a study that demonstrates that this intervention causes mood changes in any patients who have not been treated with antidepressants.
In general, several findings support the fact that depression may not be caused solely by an abnormality of 5-HT function, but more likely by a dysfunction of other systems or brain regions modulated by 5-HT or interacting with its dietary precursor. Similarly, the ATD method does not seem to challenge the 5-HT system per se, but rather triggers 5HT-mediated adverse events.
So if we cannot confirm the role of serotonin in mood and we have good reason to believe that antidepressant effect is largely based on belief, then why are we trying to “boost serotonin”?
Causing imbalances
All you have to do is spend a few minutes on
http://survivingantidepressants.org/ or
http://beyondmeds.com/ to appreciate that we have created a monster. Millions of men, women, and children the world over are suffering, without clinical guidance (because this is NOT a part of medical training) to discontinue psychiatric meds. I have been humbled, as a clinician who seeks to help these patients, by what these medications are capable of. Psychotropic withdrawal can make alcohol and heroin detox look like a breeze.
An important
analysis by the former director of the NIMH makes claims that antidepressants “create perturbations in neurotransmitter functions” causing the body to compensate through a series of adaptations which occur after “chronic administration” leading to brains that function, after a few weeks, in a way that is “qualitatively as well as quantitatively different from the normal state.”
Changes in beta-adrenergic receptor density, serotonin autoreceptor sensitivity, and serotonin turnover all struggle to compensate for the assault of the medication.
Andrews, et al., calls this “oppositional tolerance,” and demonstrate through a careful meta-analysis of 46 studies demonstrating that patient’s risk of relapse is directly proportionate to how “perturbing” the medication is, and is always higher than placebo (44.6% vs 24.7%). They challenge the notion that findings of decreased relapse on continued medication represent anything other than drug-induced response to discontinuation of a substance to which the body has developed tolerance. They go a step further to add:
“For instance, in naturalistic studies, unmedicated patients have much shorter episodes, and better long-term prospects, than medicated patients. Several of these studies have found that the average duration of an untreated episode of major depression is 12–13 weeks.”
Harvard researchers also concluded that at least fifty percent of drug-withdrawn patients relapsed within 14 months. In fact:
“Long-term antidepressant use may be depressogenic . . . it is possible that antidepressant agents modify the hardwiring of neuronal synapses (which) not only render antidepressants ineffective but also induce a resident, refractory depressive state.”
So, when your doctor says, “You see, look how sick you are, you shouldn’t have stopped that medication,” you should know that the data suggests that your symptoms are withdrawal, not relapse.
Longitudinal
studies demonstrate poor functional outcomes for those treated with 60% of patients still meeting diagnostic criteria at one year (despite transient improvement within the first 3 months). When baseline severity is controlled for, two prospective studies support a worse outcome in those prescribed medication:
One in which the never-medicated group experienced a 62% improvement by six months, whereas the drug-treated patients experienced only a 33% reduction in symptoms, and
another WHO study of depressed patients in 15 cities which found that, at the end of one year, those who weren’t exposed to psychotropic medications enjoyed much better “general health”; that their depressive symptoms were much milder”; and that they were less likely to still be “mentally ill.”
I’m not done yet. In a
retrospective 10-year study in the Netherlands, 76% of those with unmedicated depression recovered without relapse relative to 50% of those treated.
Unlike the mess of contradictory studies around short-term effects, there are no comparable studies that show a better outcome in those prescribed antidepressants long term.
First Do No Harm
So, we have a half-baked theory in a vacuum of science that that pharmaceutical industry raced to fill. We have the illusion of short-term efficacy and assumptions about long-term safety. But are these medications actually killing people?
The answer is yes.
Unequivocally, antidepressants cause suicidal and homicidal behavior. The Russian Roulette of patients vulnerable to these “side effects” is only
beginning to be elucidated and may have something to do with genetic variants around metabolism of these chemicals. Dr. David Healy has
worked tirelessly to expose the data that implicates antidepressants in suicidality and violence, maintaining a database for reporting, writing, and
lecturing about cases of medication-induced death that could make your soul wince.
What about our most vulnerable?
I have countless patients in my practice who report new onset of suicidal ideation within weeks of starting an antidepressant. In a population where there are only 2 randomized trials, I have grave concerns about postpartum women who are treated with antidepressants before more benign and
effective interventions such as dietary modification and thyroid treatment. Hold your heart as you read through
these reports of women who took their own and their childrens’ lives while treated with medications.
Then there is the use of these medications in children as young as 2 years old. How did we ever get the idea that this was a safe and effective treatment for this demographic? Look no further than data like
Study 329, which cost Glaxo Smith Klein 3 billion dollars for their efforts to promote antidepressants to children. These efforts required ghost-written and manipulated data that suppressed a signal of suicidality, falsely represented Paxil as outperforming placebo, and contributes to an irrepressible
mountain of harm done to our children by the field of psychiatry.
RIP Monoamine Theory
“Our analysis indicates that there are no specific antidepressant drugs, that most of the short-term effects of antidepressants are shared by many other drugs, and that long-term drug treatment with antidepressants or any other drugs has not been shown to lead to long-term elevation of mood. We suggest that the term “antidepressant” should be abandoned.”
So, where do we turn?
The field of
psychoneuroimmunology dominates the research as an iconic example of how medicine must surpass its own simplistic boundaries if we are going to begin to chip away at the some 50% of Americans who will struggle with mood symptoms, 11% of whom will be medicated for it.
There are times in our evolution as a cultural species when we need to unlearn what we think we know. We have to move out of the comfort of certainty and into the freeing light of uncertainty. It is from this space of acknowledged unknowing that we can truly grow. From my vantage point, this growth will encompass a sense of wonder – both a curiosity about what symptoms of mental illness may be telling us about our physiology and spirit, as well as a sense of humbled awe at all that we do not yet have the tools to appreciate. For this reason, honoring our co-evolution with the natural world, and sending the body a
signal of safety through movement, diet, meditation, and environmental detoxification represents our most primal and most powerful tool for healing.